Background
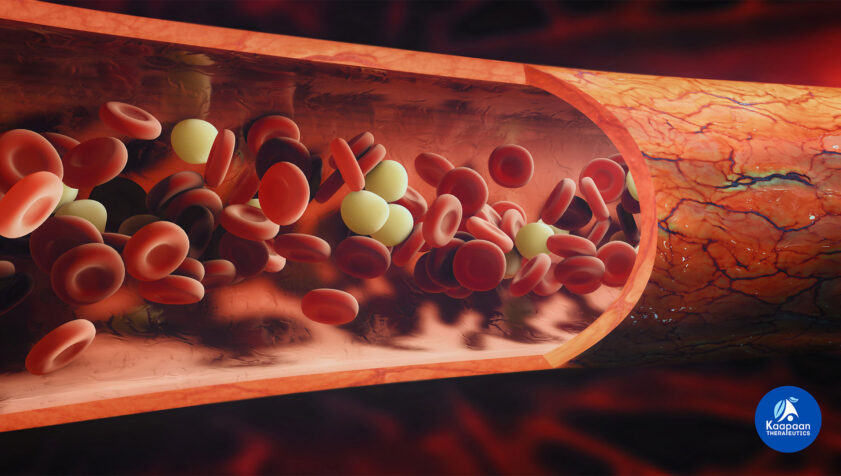
Sickle Cell Disease (SCD) is a hereditary blood disorder characterized by the production of abnormally shaped red blood cells, which can lead to various complications, including pain crises, anemia, and organ damage. Oxygen therapy, particularly Hyperbaric Oxygen Therapy (HBOT), has shown promise in managing acute complications and improving overall patient outcomes. This case study explores the application and efficacy of HBOT in treating a patient experiencing a severe sickle cell crisis.
Patient Profile
- Name: Jane Smith
- Age: 28
- Gender: Female
- Condition: Sickle Cell Disease (SCD)
- History: Jane has a history of frequent vaso-occlusive crises (VOC), chronic pain, and anemia. She presented with a severe VOC affecting multiple organs, including the lungs and kidneys.
Initial Condition
Upon admission:
- Hemoglobin Level: 6.5 g/dL (Severe anemia)
- Oxygen Saturation: 88% on room air
- Symptoms: Severe pain (VAS score 9/10), shortness of breath, fatigue, jaundice, and hematuria.
- Complications: Acute chest syndrome, acute renal insufficiency.
Treatment Plan
A comprehensive approach was adopted, combining conventional treatment for SCD with HBOT to manage the acute crisis.
- Initial Stabilization:
- Intravenous fluids
- Pain management with opioids
- Blood transfusion
- Antibiotics for suspected infection
- Hyperbaric Oxygen Therapy (HBOT):
- Regimen: 90-minute sessions at 2.0 ATA (atmospheres absolute), twice daily for the first 3 days, then once daily for the next 7 days.
- Objective: To increase oxygen delivery to tissues, reduce sickling of red blood cells, alleviate pain, and improve organ function.
Progress and Observations
Day 1-3:
- Pain Management: Significant reduction in pain (VAS score decreased to 5/10).
- Oxygen Saturation: Improved to 95% on room air.
- Clinical Signs: Reduced shortness of breath, improved energy levels, and decreased jaundice.
Day 4-7:
- Hemoglobin Level: Increased to 8.0 g/dL.
- Oxygen Saturation: Stable at 97% on room air.
- Clinical Signs: Further reduction in pain (VAS score 3/10), normalization of urine color, improved renal function.
Day 8-10:
- Hemoglobin Level: Stabilized at 9.0 g/dL.
- Oxygen Saturation: Consistently above 97% on room air.
- Clinical Signs: Pain nearly resolved (VAS score 1/10), normal breathing, no signs of jaundice, stable renal function.
Outcome
By the end of the 10-day HBOT regimen:
- Hemoglobin Level: 9.5 g/dL
- Functional Status: Jane experienced significant relief from her acute vaso-occlusive crisis, with substantial improvement in pain levels, oxygen saturation, and overall well-being. She was discharged with a plan for regular follow-up and continued management of her SCD.
Discussion
This case of Jane Smith highlights the potential benefits of Hyperbaric Oxygen Therapy in managing acute complications of Sickle Cell Disease. HBOT helped increase oxygen delivery to tissues, reduce the sickling of red blood cells, and improve overall organ function, which contributed to the resolution of her vaso-occlusive crisis. While HBOT is not a cure for SCD, its use as an adjunctive therapy during acute crises can significantly improve patient outcomes.
Conclusion
This case study supports the use of Hyperbaric Oxygen Therapy as an adjunctive treatment for acute vaso-occlusive crises in patients with Sickle Cell Disease. Further research and clinical trials are recommended to establish standardized protocols and to better understand the mechanisms by which HBOT aids in the management of blood-related illnesses.
This case study is a hypothetical example designed to illustrate the potential benefits of HBOT in treating blood-related illnesses, specifically Sickle Cell Disease. It is not based on a real patient case but reflects current medical understanding and research on the topic.